RADIOLOGY REIMBURSEMENT & CODING
Series: Radiology Reimbursement & Coding
This webinar series is designed to help billers, coders, practice administrators and radiologists stay on top of the rapidly changing reimbursement environment. Each session delivers practical information to help you ensure correct coding, capture necessary information in radiology reports and remain in compliance.
AUC 301: Get Ready for 2020 – a Coding and Compliance Perspective

Serena Sardo
Manager of Radiology Coding Compliance
This webinar is designed to help billing and coding staff prepare for the upcoming changes related to Appropriate Use Criteria (AUC). It will review some of the background behind AUC, terminology, and other key ingredients for a successful adoption of this CMS program.
September 26, 2019 AUC 301 Recorded Webinar
AUC 201: Integrating Your Site with vRad to Ensure Required Data Transfer

Serena Sardo
Manager of Radiology Coding Compliance
vRad clients need to prepare for the data sharing that will be necessary to avoid payment denials under Appropriate Use Criteria (AUC). This webinar teachs clients how to create a seamless transition for them and their facilities. It will cover key components of AUC, review deadlines, and discuss the various options for supplying G-Codes and Modifiers to vRad.
September 12, 2019 AUC 201 Recorder Webinar
AUC 101: Understanding the impact of AUC and vRad's preparedness program

Katie Schoenberger
Sr. Director of Payer Services

Serena Sardo
Manager of Radiology Coding Compliance
This webinar discusses Appropriate Use Criteria (AUC) within the industry. In addition, it outlines vRad’s mission, vision, and goals on how they will use AUC within the business to ensure a seamless transition for clients and their facilities.
August 22, 2019 AUC 101 Recorded Webinar
Avoid Radiology Claim Denials with Effective Medical Necessity Documentation

Sharon Roeder, BA, CPC
Director of Medical Coding and Compliance
Lack of clinical documentation in the radiology order is a primary contributor to inadequate medical necessity documentation, which can result in denied claims and compliance concerns.
Claim denials can be avoided by educating radiologists and radiology support staff on the critical role they play in the coding and reimbursement process.
Watch this webinar recording to better understand how to document the medical necessity details in radiology orders and reports.
Avoid Payment Denial: Key Steps to Prepare for AUC (Appropriate Use Criteria)
Shannon Roeder, BA, CPC
Director of Medical Coding Compliance
The Protecting Access to Medicare Act will require referring providers to consult appropriate use criteria (AUC) prior to ordering advanced diagnostic imaging services (CT, MR, nuclear medicine exams and PET). The burden of reporting the AUC consultation is on the radiologist, whose payment will be denied in full when the ordering provider fails to use the system.
Register today for this informative webinar to learn about the AUC rule and get a jump start on your preparation for the January 1, 2020 implementation date. Sharon will highlight the guidance CMS has provided in the 2016, 2017, and 2018 final rules and how this regulation will impact radiologists.
Survive 2018 Coding and Medicare Payment Policy Updates for Radiology – Tips and Tools to Thrive
Sharon Roeder
Wendi Krumm
Join this webinar to ensure your practice has prepared for the coding and billing changes for 2018, including the changes made by the (MPFS) Final Rule. This webinar will highlight key financial and operational impacts to radiology services.
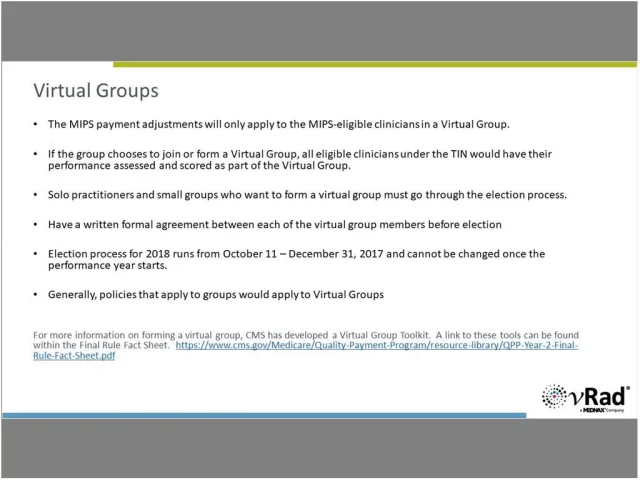
Survive Year 2 of the Quality Payment Program – Tips and Tools to Thrive
Is your practice prepared to thrive under the new Quality Payment Program? How will your performance compare to your peers? 2018 is year 2 of the Quality Payment Program and CMS is raising the stakes – posing a significant challenge to healthcare organizations. This year the MIPS incentive and penalty percentages are increasing to +/-5%, and the performance threshold is being raised from 3 to 15. Are you prepared? Join this webinar to understand what your practice can do to maximize incentives and minimize penalties under the Quality Payment Program. The webinar compares the differences between the 2017 and 2018 requirements of the Merit-based Incentive Payment System (MIPS) and provides many helpful tools.
2017 CPT® Changes for Radiology
Understanding 2017 coding changes is crucial to obtaining accurate reimbursement for radiology services provided. The breast imaging section of CPT® was revised ‒ will Medicare process these new codes in 2017? 2018? Other changes in 2017 impact ultrasound, dialysis graft/fistula imaging and interventions, angioplasty radiology services and billing for moderate sedation administration. Radiologists and coders will also need to understand revisions to the NCCI Policy Manual for 2017. We provide information from the CMS Final Rules pertinent to radiology practices including the new modifier for the drug discarding policy. CPT Copyright 2017 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
What You Need to Know About the Merit-Based Incentive Payment System (MIPS) Part 1 & Part 2
Part 1: Overview, Participation & Reporting, Performance & Scoring Part 2: Quality Measures and Improvement Activities Categories MIPS Tips
Obstetrical and Non-Obstetrical Pelvic Ultrasound Exams
Pelvic ultrasound studies present documentation challenges for radiology departments and practices. Are you leaving money on the table because you are inadequately documenting these studies? Are you looking for tips to improve capturing the required elements for these exams? This presentation walks you through documentation requirements for Obstetrical and Non-Obstetrical ultrasound procedures and arms you with the information needed to maximize reimbursement and reduce your compliance risks.
Improving Reimbursement with Accurate Radiology Documentation
This session reviews the documentation requirements for common radiology procedures. You’ll also learn valuable tips on educating providers and staff about the documentation necessary to reduce burdensome report addendums, ensure accurate billing, and improve reimbursement.
Preparing for ICD-10-CM: Are You Ready for Implementation? It's Not Too Late.
This presentation will provide ideas and tools for capturing clinical details from referring physicians. Getting the level of detail from the ordering physicians to the final radiology reports will be critical for maximum and timely reimbursement.
Nuclear Medicine Dictation Standards
Obtain accurate reimbursement by knowing what documentation to look for.
Fluoroscopic Guidance Criteria
Determine when fluoroscopic guidance can be reported.
Capturing Critical Elements in Ultrasound Reports
Learn the most common reason for addendum requests.
Documentation for Rendering 3D Imaging
Understand how to document computed tomographic angiography (CTA) studies and concurrent supervision of 3D reconstruction.


