CME Preferences and Perspectives Among Practicing Radiologists
Journal Name: Clinical Imaging
Published: 02/01/2025

Remote radiologist jobs with flexible schedules, equitable pay, and the most advanced reading platform. Discover teleradiology at vRad.

Radiologist well-being matters. Explore how vRad takes action to prevent burnout with expert-led, confidential support through our partnership with VITAL WorkLife. Helping radiologists thrive.

Visit the vRad blog for radiologist experiences at vRad, career resources, and more.

vRad provides radiology residents and fellows with free radiology education resources for ABR boards, noon lectures, and CME.

Teleradiology services leader since 2001. See how vRad AI is helping deliver faster, higher-quality care for 50,000+ critical patients each year.
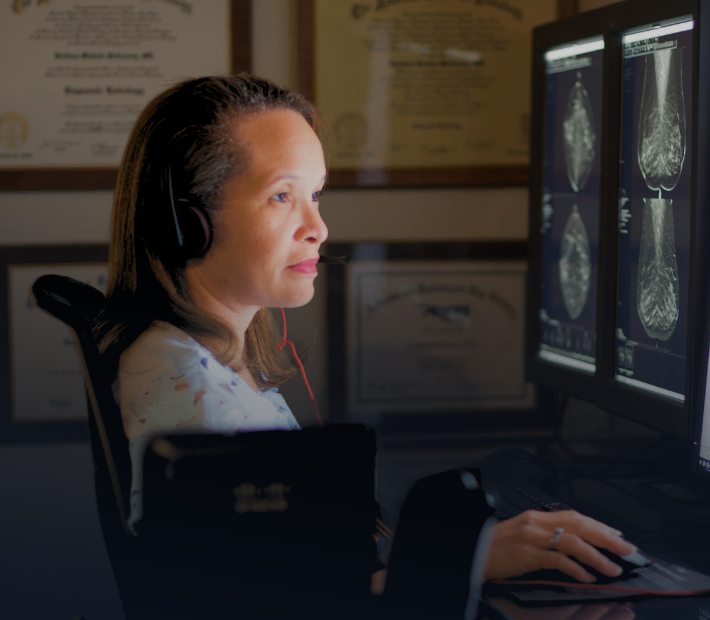
Subspecialist care for the women in your community. 48-hour screenings. 1-hour diagnostics. Comprehensive compliance and inspection support.
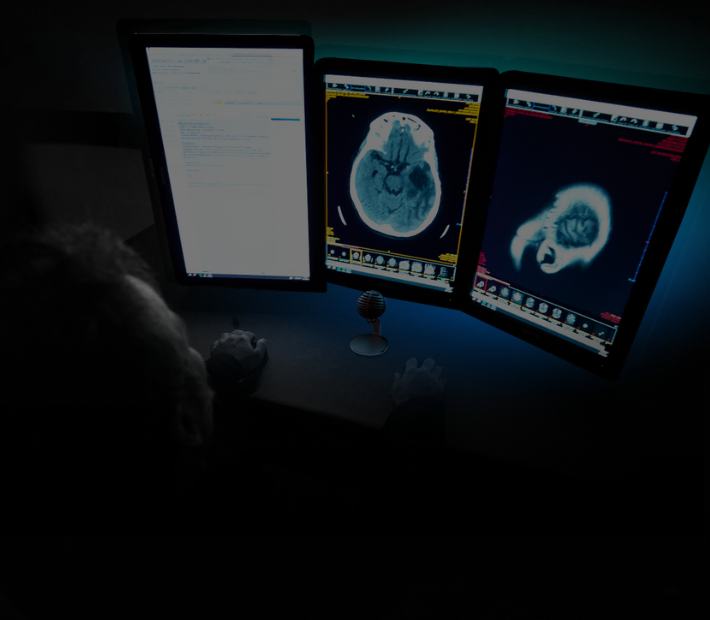
vRad’s stroke protocol auto-assigns stroke cases to the top of all available radiologists’ worklists, with requirements to be read next.

vRad’s unique teleradiology workflow for trauma studies delivers consistently fast turnaround times—even during periods of high volume.

vRad’s Operations Center is the central hub that ensures imaging studies and communications are handled efficiently and swiftly.

vRad is delivering faster radiology turnaround times for 40,000+ critical patients annually, using four unique strategies, including AI.

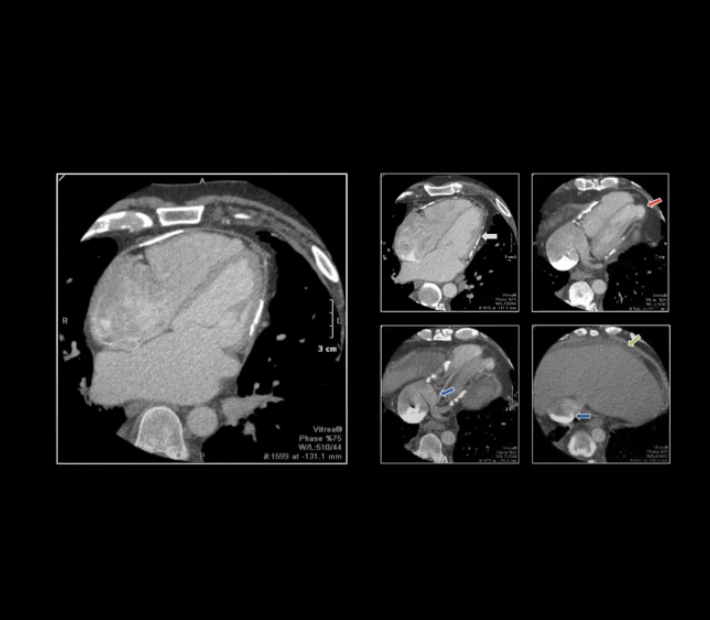
vRad is developing and using AI to improve radiology quality assurance and reduce medical malpractice risk.

Now you can power your practice with the same fully integrated technology and support ecosystem we use. The vRad Platform.

Since developing and launching our first model in 2015, vRad has been at the forefront of AI in radiology.
Since 2010, vRad Radiology Education has provided high-quality radiology CME. Open to all radiologists, these 15-minute online modules are a convenient way to stay up to date on practical radiology topics.

Join vRad’s annual spring CME conference, featuring top speakers and practical radiology topics.

vRad provides radiology residents and fellows with free radiology education resources for ABR boards, noon lectures, and CME.

Academically oriented radiologists love practicing at vRad too. Check out the research published by vRad radiologists and team members.

Learn how vRad revolutionized radiology and has been at the forefront of innovation since 2001.



Visit the vRad blog for radiologist experiences at vRad, career resources, and more.

Explore our practice’s reading platform, breast imaging program, AI, and more. Plus, hear from vRad radiologists about what it’s like to practice at vRad.

Ready to be part of something meaningful? Explore team member careers at vRad.

Author: Christine Lamoureux, Eric Rohren, Edward Callaway, Erin Vair-Grilley, Scott G. Baginski, Phil Ramis, Tarek N. Hanna
Journal Name: Clinical Imaging
Published: 02/01/2025
Author: Eric Chang, Stephane Desouches, Lauren Ladd, Hyojeong Lee, Catherine Roberts, Vanessa Zayas-Colon
Journal Name: American College of Radiology
Published: 12/06/2023
Author: Shannon Zhou, Tarek Hanna, Tianwen Ma, Timothy Johnson, Christine Lamoureux, Scott Weber, Jamlik-Omari Johnson, Scott Steenburg, Jeffrey Dunkle, Suzanne Chong
Journal Name: Emergency Radiology
Published: 07/31/2023
Author: Christine Lamoureux, Tarek Hanna, Edward Callaway, Michael Bruno, Scott Weber, Devin Sprecher, Timothy Johnson
Journal Name: Emergency Radiology
Published: 07/17/2023
Author: Robert Harris, Scott Baginski, Yulia Bronstein, Dietrich Schultze, Kenneth Segel, Shwan Kim, Jerry Lohr, Steve Towey, Nishit Shahi, Ian Driscoll, Brian Baker
Journal Name: Spine
Published: 01/01/2023
Author: Sarah Thomas, Tyler Fraum, Lawrence Ngo, Robert Harris, Elie Balesh, Mustafa Bashir, Benjamin Wildman-Tobriner
Journal Name: Journal of the American College of Radiology
Published: 11/01/2022
Author: Catherine Roberts, Darlene Metter, Michael Fox, Marc Appel, Shari Jawetz, William Morrison, Nicholas Nacey, Nicholas Said, James Stensby, Naveen Subhas, Katherine Tynus, Eric Walker, Joseph Yu, Mark Kransdorf
Journal Name: Journal of the American College of Radiology
Published: 05/01/2022
Author: Yiting Xie, Benedikt Graf, Parisa Farzam, Brian Baker, Christine Lamoureux, Arkadiusz Sitek
Journal Name: SPIE Medical Imaging
Published: 04/04/2022
Author: Suzanne Chong, Tarek Hanna, Christine Lamoureux, Tianwen Ma, Scott Weber, Jamlik-Omari Johnson, Eric Friedberg, Robert Pyatt Jr., Catherine Everett, Timothy Johnson
Journal Name: American Journal of Roentgenology
Published: 10/25/2021